Individualized Pelvic Health Treatment for Menopause
Symptoms like menopause-related vaginal itching, leaking urine, painful penetrative sexual intercourse, aching joints, and back pain during perimenopause can begin during perimenopause and continue into postmenopause. These changes are often related to hormonal shifts, including decreased estrogen.
Estrogen supports blood flow, tissue elasticity, joint lubrication, and appropriate mucus production for pelvic tissues. When estrogen fluctuates or declines, people may notice joint pain as a perimenopause symptom, stiffness upon waking, low back discomfort, pelvic pain, or changes in bladder and sexual function. Consulting with us can help you understand your options for vulvar health, pelvic floor support, and whole-body movement during this transition.
Pelvic floor physical therapy can help improve circulation to muscles and connective tissue so available hormone levels are better supported. It can also help you coordinate your pelvic floor with breath, posture, and core movement to improve bladder function, sexual comfort, and overall mobility. If you are experiencing aching joints during perimenopause or back pain that feels persistent or unfamiliar, retraining how your body moves and loads through daily activities can make a meaningful difference.
Would you like to enjoy orgasm and feel confident with penetrative sex? Connecting more deeply with your pelvic floor muscles—without forcing or overworking them—can help support comfort, pleasure, and ease.
“Kegels” is not a descriptive term
Pelvic floor muscles, like any muscle group, are healthiest when they embody awareness, flexibility, strength, relaxation, coordination, power, and endurance—and when they are not always sore to the touch. During perimenopause, tissues may respond differently to load, stress, and exercise, which can contribute to joint pain, back pain, or pelvic discomfort if movement patterns are not well supported.
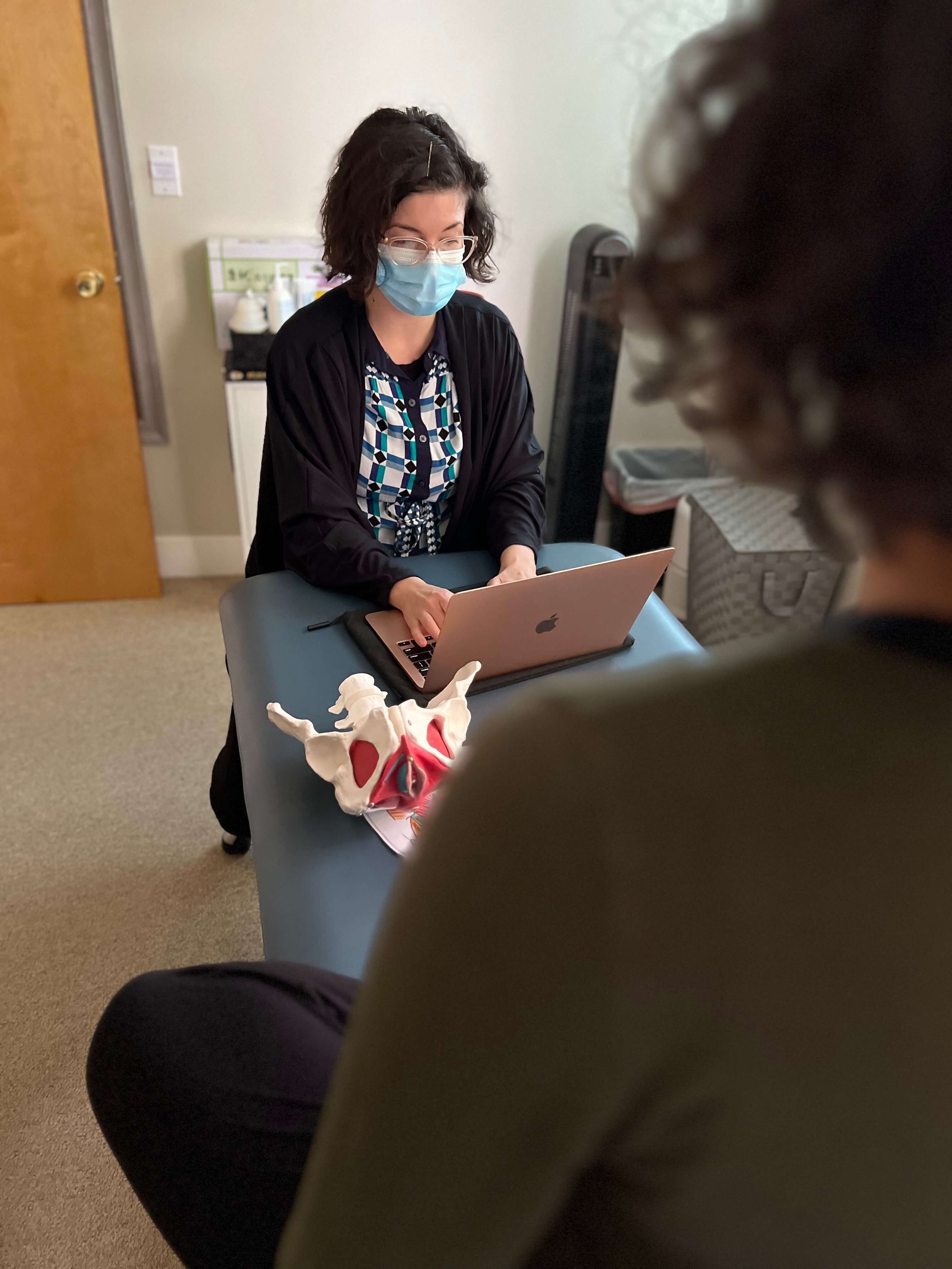
A pelvic health physical therapist uses skilled techniques to help you learn pelvic floor exercises that are specific to your needs, and to integrate pelvic floor support into functional movements, total-body exercise, and repetitive daily tasks. This approach supports not only bladder and sexual health, but also how your spine, hips, and joints move during perimenopause.
Feel confident in your body and empowered with pelvic education
At Bodyful, our clients begin to notice changes in their symptoms—and gain a clear map for how to integrate pelvic health into their daily life—often by the first visit. For many people navigating perimenopause, this includes understanding how hormonal shifts may relate to joint pain, back pain, pelvic floor symptoms, and changes in recovery.
Typically, strength gains and specialized neuromuscular training require a commitment of about 10–12 weeks. After your first visit, you will receive a detailed, individualized plan so you can begin moving with confidence and independence, using a consistent home practice that supports both your nervous system and your joints.
What is the definition of menopause?
Menopause is defined as the point when your period has ended consistently for 12 months.
When does menopause start?
The average age is 51. Perimenopause symptoms—including joint pain, aching joints, back pain, pelvic discomfort, and changes in bladder or sexual function—can begin up to ten years earlier.