What Causes Bladder Pain Without Infection?
Authored by Bodyful Physical Therapy and Wellness
Understanding Bladder Pain (When There’s No Infection)
Do you feel like you have to pee all the time?
Do you feel a constant sensation of a full bladder, even right after you go?
Do you feel burning when peeing, especially after sex?
Have you been told you “can take antibiotics just in case” but your urine culture tests keep coming back negative?
These are common experiences for people with bladder pain without infection.
In this blog, you’ll learn:
7 reasons you can feel bladder pain, urgency, or burning without a UTI
3 ways you can begin shifting symptoms now
Why movement-based pelvic floor therapy can help you stop cycling through unnecessary antibiotics
Why You Can Have Bladder Pain Without a UTI
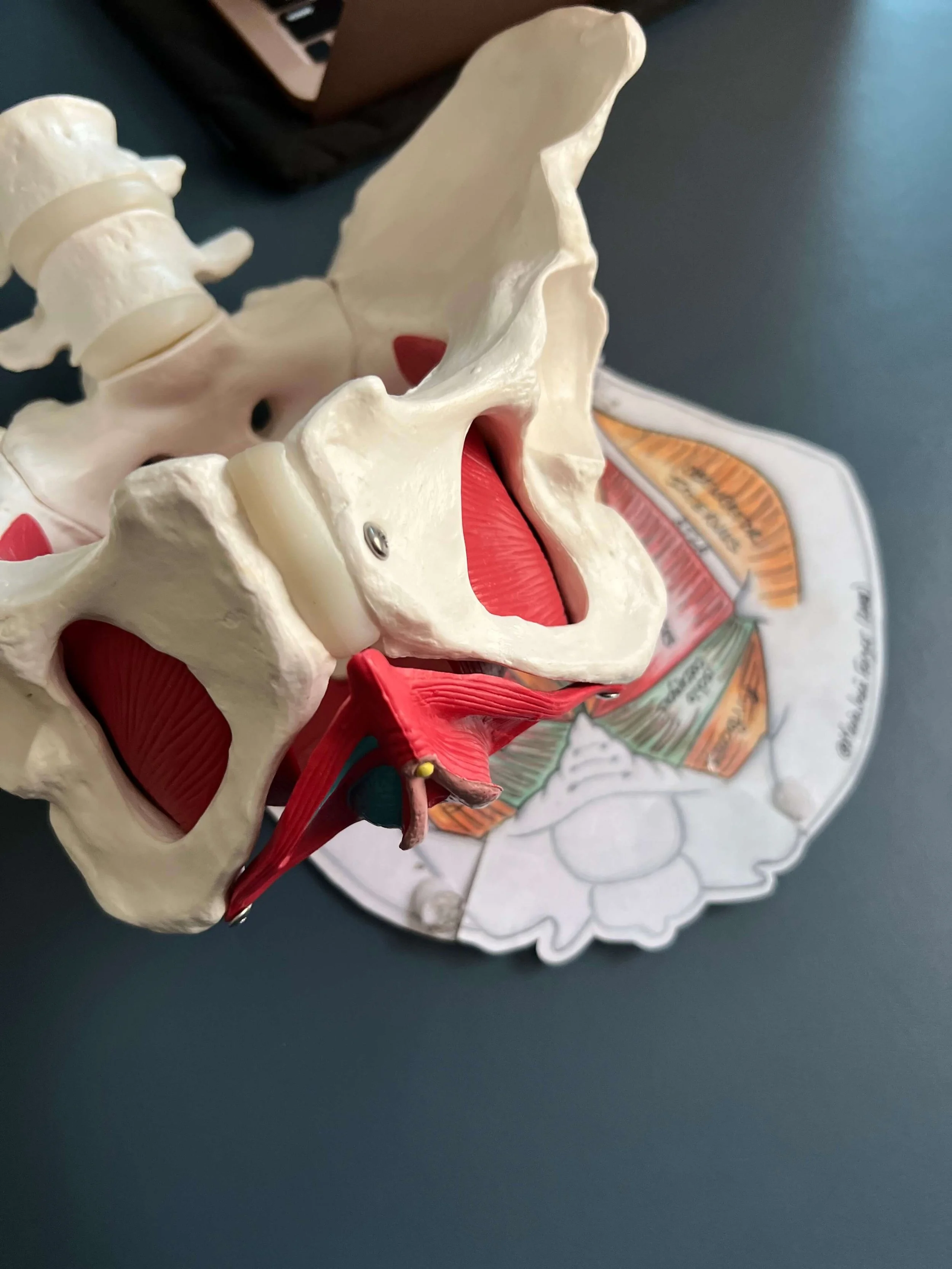
1. Over-Recruited Front Pelvic Floor Muscles (Urethral Tension)
Your bladder and urethra are deeply influenced by the muscles and fascia of the pelvic floor.
At the front of the pelvis is a group of muscles called the urogenital triangle/superficial pelvic floor muscles. These muscles help:
keep urine in when you don’t want to pee
relax when it’s time to empty your bladder
When these muscles are gripping or tense, they can:
pull on the urethra
create a false urge to pee all the time
cause burning with urination, especially after sex
This is a common contributor to:
feeling like you always have to pee
burning pee after sex
UTI-like symptoms with negative tests
One surprising contributor? Your feet.
If you habitually bear weight into the front of your feet, this can increase activation of the front pelvic floor muscles, changing how tension is absorbed throughout the pelvis.
2. Obturator Internus Tension (Hip–Bladder Connection)
The obturator internus is a deep hip joint muscle that is also continuous with the back wall of the pelvic floor.
This muscle has direct fascial connections to the bladder and urethra.
Clinically, bladder urgency, burning, and pressure can be:
recreated by tension in this muscle
reduced when it is integrated into your pelvic health as sufficient hip stabilizing muscle
This helps explain why bladder symptoms can feel worse:
after sitting
after sex
with hip tightness or pelvic pain
If this muscle is overworking, it’s essential to assess:
hip mobility
pelvic control and spinal elongation during repetitive functional activities
pelvic floor muscle coordination
3. Chronic Abdominal Wall Holding or Gripping (“Sucking In”)
If you constantly hold tension in your abdomen—whether from “good” posture, stress, or “core” training—it can affect your bladder.
Your bladder is held by the pelvic bowl and is connected to the abdominal fascia.
When the abdominal wall grips and you hold your breath often when exerting effort:
blood flow decreases
nerves become more irritable
pressure increases on the bladder from muscle strain
This can contribute to:
bladder sensitivity
urgency
burning sensations
Learning how to embody core support with coordinated breathing and sufficient hip mobility and strength can significantly reduce bladder irritation.
4. Insufficient Abdominal Pressure Management
Postures such as:
forward head
rounded shoulders
abdominal gripping at ribs
stiff low back and hips
can increase strain onto the pelvic organs.
When this posture continues during:
lifting
bending
exercise
daily tasks
the bladder can become more stressed and tissues around it can become sensitive.
Abdominal pressure management is a core part of pelvic floor physical therapy for bladder urgency and pain without infection.
5. History of Recurrent UTIs or Infections
If you’ve had real bladder infections in the past, your nervous system may still be on high alert—even after the infection has resolved.
Chronic inflammation can sensitize pain-sensing nerve fibers (C-fibers), meaning:
many sensations start to feel painful
urgency and burning persist without a pathogen
This is not “in your head.”
It’s neurophysiology.
Somatic pelvic floor therapy works directly with these nervous system patterns to help your body relearn safety.
6. Bladder & Bowel Habits That Reinforce Urgency
Do any of these sound familiar?
Peeing “just in case”
Urinating every hour or less
Stream shorter than ~8 seconds
Constipation or straining
Drinking alcohol
These habits can train the bladder into urgency and hypersensitivity.
Bladder perception is very responsive to environmental triggers and our habits.
7. Spinal & Neural Tension
All bladder nerves originate near the spine.
Restrictions anywhere along the nerve pathway—from below the ribs to the bladder—can increase neural tension, contributing to:
urgency
burning
bladder fullness
sensitive urethra
Targeted movement can restore mobility and reduce nerve irritation.
What You Can Try Right Now
Here are three gentle practices to begin calming bladder sensitivity:
1. Diaphragmatic Breathing
Place your hands on the sides of your rib cage.
Breathe into the ribs, letting your belly stay soft.
Avoid gripping or pushing.
2. Child’s Pose (Supported)
Use pillows or bolsters so your body feels fully supported.
Breathe into your ribs and feel your breath pressure flow to your pelvic floor and tailbone.
3. Somatic Imagery
Place or hover your hands below your belly button.
Imagine your bladder as something soft and fluid—like a jellyfish—moving gently with your breath.
Pause. Does your breath change?
You Are Not Broken
Bladder urgency, burning after sex, and the feeling of a constantly full bladder are real experiences with real explanations—even when tests are negative.
Your body is asking for a change.
There are different ways to move, to breathe, to get stronger, to improve your symptoms with a consistent practice.
If you’re ready for individualized support, pelvic floor therapy can help you identify what’s driving your symptoms and guide sustainable change.
Bodyful Physical Therapy and Wellness is located in Oakland, CA, offering in-person care throughout the Bay Area and telehealth across California. Virtual somatic wellness sessions are also available.
You deserve relief—and options beyond antibiotics.